Andrew Siegel MD 7/20/2019
“Radical prostatectomy” is the surgical removal of the entire prostate and the attached seminal vesicles. Upon excision, the detached urethra is sewn to the bladder neck to restore the continuity of the lower urinary tract. The goal is cancer control and preservation of urinary and sexual function. At the time of the prostatectomy, pelvic lymph nodes are usually sampled, a consideration for any man undergoing radical prostatectomy and a definite recommendation for those with unfavorable intermediate risk or high risk features. A pathologist microscopically examines the removed tissues and provides valuable information as to the precise pathological stage of the prostate cancer. Before the availability of laparoscopy and robotics, prostatectomy was performed through large incisions—either retro-pubic (a lower abdominal incision) or perineal (an incision between the scrotum and anus)—with poorer visualization, more blood loss, less precision, more pain and longer hospital stays and recovery. With technical advances, the laparoscopic approach replaced the open technique, and more recently, the robot has further refined the laparoscopic approach.
Robotic-Assisted Laparoscopic Prostatectomy (RALP)
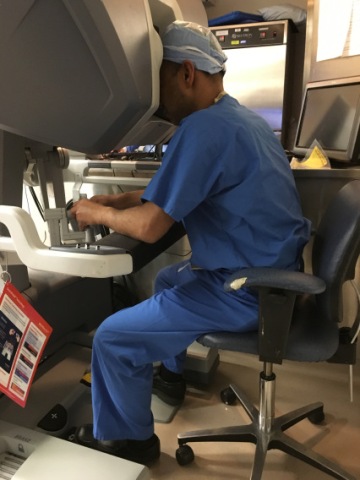
Dr. M. Ahmed at console performing RALP; observe hands on joysticks and feet on pedals
With the advent of laparoscopy (“keyhole”) surgery done via small portals and thereafter the development and refinement of surgical robotics, many advantages have accrued. Major surgical procedures are performed less invasively, with a reduction in blood loss, a brighter, sharper and magnified visual field for the surgeon, refined precision in the dissection of delicate tissue and facilitation of suturing. The urologist with a dedicated team of assistants harnesses the powers and advantages of robotic technology -– an extraordinary example of human-machine symbiosis.
Initially, portals are placed via small incisions. As opposed to large incisions, these keyholes leave only small scars and cause limited pain. Through one of these portals, a camera is inserted to obtain an optically magnified, three-dimensional, high definition view of the surgical field. The camera can be manipulated, zoomed, rotated, etc. Robotic instruments that are mounted on the robot’s arms are inserted through the portals. These include electric cautery (used to cut and coagulate tissue), scissors, forceps, scalpels, needle holders and other surgical tools.
In our practice, two board-certified urologic surgeons perform the surgery. One surgeon sits at a console remote from the patient and controls and maneuvers the robotic instruments while viewing the operation in real-time, while the other surgeon is positioned on the side of the patient and assists with instrument exchanges and aids in the dissection. An advantage of sitting at the console is that it is a comfortable, ergonomically favorable position that minimizes postural fatigue that often accompanies standing up for traditional open surgery. The surgeon’s fingers are inserted into surgical joysticks that provide control of the instruments by using natural hand and wrist movements, with the system converting the surgeon’s movements to precise, tremor-free robotic micro-movements. In addition to hand controls, the surgeon uses foot pedals to control the camera, focus, electrocautery and coagulation. Seven degrees of freedom (each direction a joint can move is a degree of freedom) are provided at the instrument tips. 540 degrees of pivoting (a full 360-degree rotation plus an additional 180-degree rotation) provide greater maneuverability than is possible with human hands or laparoscopic instruments.
RALP is currently the surgical approach of choice for removing a cancerous prostate gland due to the aforementioned refinements it provides in comparison to open and traditional laparoscopic surgery. Because of these advantages, in addition to less bleeding, less post-operative pain and shorter hospital stays, there are improved outcomes in terms of urinary control and sexual function as compared with the open approach.
RALP generally entails several hours under anesthesia and an overnight stay in the hospital. A catheter typically remains in the bladder for a week or so after the surgery. A unique benefit of RALP is that the removed tissue is available to be scrutinized in its entirety by the pathologist. The pathology report on the removed prostate, seminal vesicles, and lymph nodes provides important information regarding prognosis and helps determine if any other forms of therapy are indicated.
If the pathology report indicates that the cancer is all contained within the prostate capsule with normal margins, the prognosis is excellent with a high likelihood of cure of the localized prostate cancer. Our goal as urologists is the achievement of a “trifecta”—an undetectable PSA, excellent urinary control and satisfactory erections.
Possible adverse pathological features include the following:
- Peri-neural invasion or lymphatic-vascular invasion (growth of the cancer along the nerve, lymphatic or blood vessel branches)
- Extra-capsular extension (extension of the cancer beyond the prostate capsule)
- Positive surgical margins (cancer at the specimen edge)
- Seminal vesicle invasion (invasion into the seminal vesicles)
- Lymph node metastases (spread to the lymph nodes)
Depending on what, if any, adverse features may be present, additional therapies may be required to treat the prostate cancer. More about this in a forthcoming entry.
Advantages of RALP:
- A one-time procedure that intends to completely remove the cancerous organ and offers excellent long-term cancer control
- The pathology report on the removed prostate and sampled lymph nodes will offer staging and prognostic information
- Provides an excellent means of managing lower urinary tract symptoms due to benign prostate enlargement and prevents the future occurrence of symptomatic benign prostate enlargement, common in the aging male
- PSA should be undetectable after the procedure, so recurrences are easy to detect if PSA becomes detectable
- If RALP fails to cure the cancer, radiation therapy is available as a backup, potentially curative option
- The major complications, erectile dysfunction and urinary incontinence, are treatable
Disadvantages of RALP:
- A technically challenging, major operation that requires anesthesia, a hospital stay, a catheter and time lost from normal activities
- Potential over-treatment of low risk cancers
- Potential for adverse pathological findings that may require subsequent radiation therapy
- 20-25% will have a PSA recurrence, indicative of a limitation of surgery to cure the cancer in all cases
- Possibility of rectal injury, erectile dysfunction and urinary incontinence
- Dry ejaculation
- Possibility of penile shortening
- Possibility of bladder neck contracture—scar tissue where the bladder neck is sewn to the urethra, which may necessitate further procedures (but much less occurrence with robotic approach as opposed to open approach)
Wishing you the best of health,
![]()
A new blog is posted weekly. To receive a free subscription with delivery to your email inbox visit the following link and click on “email subscription”: www.HealthDoc13.WordPress.com
Dr. Andrew Siegel is a physician and urological surgeon who is board-certified in urology as well as in female pelvic medicine and reconstructive surgery. He is an Assistant Clinical Professor of Surgery at the Rutgers-New Jersey Medical School and is a Castle Connolly Top Doctor New York Metro Area, Inside Jersey Top Doctor and Inside Jersey Top Doctor for Women’s Health. His mission is to “bridge the gap” between the public and the medical community. He is a urologist at New Jersey Urology, the largest urology practice in the United States.
The content of this entry is excerpted from his new book, PROSTATE CANCER 20/20: A Practical Guide to Understanding Management Options for Patients and Their Families

Video trailer for Prostate Cancer 20/20
Preview of Prostate Cancer 20/20
Andrew Siegel MD Amazon author page
Prostate Cancer 20/20 on Apple iBooks
Dr. Siegel’s other books:
PROMISCUOUS EATING— Understanding and Ending Our Self-Destructive Relationship with Food
MALE PELVIC FITNESS: Optimizing Sexual and Urinary Health
THE KEGEL FIX: Recharging Female Pelvic, Sexual, and Urinary Health
Tags: Andrew Siegel MD, prostate cancer, Prostate Cancer 20/20, radical prostatectomy, RALP, robotic-assisted laparoscopic prostatectomy
July 27, 2019 at 11:45 AM |
[…] Maximizing our health by promoting wellness; bridging the knowledge gap between physicians and the community. « Robotic-Assisted Surgical Removal of the Prostate: What You Need to Know […]
August 3, 2019 at 7:18 AM |
[…] after robotic-assisted laparoscopic prostatectomy (RALP) should be and most often is undetectable, meaning zero. However, it is conceivable that prostate […]
October 19, 2019 at 6:32 AM |
[…] are alternatives to radical prostatectomy and radiation therapy as treatment for prostate cancer. Focal ablative therapies use different […]
December 7, 2019 at 7:02 AM |
[…] battlegrounds and can work separately or in tandem to keep the enemy at bay. One can think of surgery (RALP) as the Army with its ground forces using artillery and tactical weapons to mount a direct attack […]
December 28, 2019 at 6:40 AM |
[…] Robotic assisted laparoscopic prostatectomy (RALP) is the surgical standard of care for the surgical management of prostate cancer. The newest robotic innovation is single port robotic surgery. Used in select cases, instead of multiple keyhole incisions in the abdomen that are used in traditional RALP, this breakthrough technology uses a single incision near the belly button. Within this single port of entry into the body are introduced the endoscopic instruments and camera. This new method of reducing surgical access points and the capability of performing complex maneuvers in smaller spaces compared with multiport procedures has the potential to result in less pain, less scarring, and shorter hospital stays. […]
March 7, 2020 at 9:56 AM |
[…] Urinary Problems After Radical Prostatectomy […]
March 14, 2020 at 6:55 AM |
[…] most cases, urinary leakage that occurs with sexual activity happens as a consequence of surgical removal of the cancerous prostate gland. Incontinence can occur with sexual stimulation, with sexual intercourse and/or with sexual […]
April 4, 2020 at 6:36 AM |
[…] simple and conservative approach to help resume bladder control (and erections) following radical prostatectomy. Stress urinary incontinence—leakage with sports, coughing, sneezing, bending and other high […]
May 2, 2020 at 7:05 AM |
[…] of the disease often become the side effects of treatment. The most common complications after radical prostatectomy are sexual dysfunction and urinary incontinence, quality of life issues that may be less well […]
May 9, 2020 at 6:47 AM |
[…] Radical prostatectomy […]
August 1, 2020 at 6:53 AM |
[…] causes sexual dysfunction, but rather the side effects of the treatment. Patients who undergo surgery, radiation, androgen deprivation therapy and focal ablative therapies commonly experience […]
September 12, 2020 at 7:02 AM |
[…] be an effective means of treating ED and is also helpful in the penile rehabilitative process after prostatectomy to maintain penile blood flow and keep the erectile tissues supple and elastic. It also can be […]
January 23, 2021 at 5:36 AM |
[…] with localized prostate cancer have a choice between active surveillance and active treatments (surgery, radiation, androgen deprivation, focal therapies). Active treatments increase survival and […]
February 6, 2021 at 6:17 AM |
[…] cancerous prostate was surgically removed using the state-of-the-art laparoscopic robotic nerve-sparing technique by a highly skilled and experienced urologist. With the cancer concerns gone and the PSA […]
February 13, 2021 at 5:54 AM |
[…] cancerous prostate was surgically removed using the state-of-the-art laparoscopic robotic nerve-sparing technique by a highly skilled and experienced urologist. With the cancer concerns gone and the PSA […]
May 22, 2021 at 5:38 AM |
[…] the prostate as treatment for prostate cancer (robotic assisted laparoscopic prostatectomy) may result in penile shortening. The gap in the urethra after prostate removal is bridged by sewing […]
April 27, 2024 at 6:51 AM |
[…] it is even more important for the follow-up of prostate cancer patients following treatment. After robotic assisted laparoscopic prostatectomy (RALP), with the prostate surgically removed, the expected PSA level should drop precipitously and be […]